Cervical biopsy: fundamentals, techniques, and relevance in screening and early diagnosis of cervical cancer
DOI:
https://doi.org/10.5327/2237-4574-2024820019Keywords:
cancer, cervix, biopsyAbstract
Cervical cancer is a prevalent disease with a significant impact on public health globally, especially in low- and middleincome countries, where the majority of related deaths occur. Cervical biopsy stands out as an effective method for early
diagnosis of this disease, allowing for the identification of precursor and invasive lesions, thus enabling timely interventions.
Different techniques can be used, such as the biopsy with a punch forceps and the rotary curette of Baliu, which have distinct
characteristics in terms of depth of the tissue sample, precision, and bleeding, with the choice depending on the clinical case
and the experience of the colposcopist. Cone resections of the cervix (LEEP and conization) and curettage of the canal are
also considered biopsy procedures, as they can also provide a diagnosis when indicated. In Brazil, the persistence of high
morbidity and mortality from cervical cancer underscores the need for more effective screening strategies and expanded access
to diagnostic and therapeutic interventions, highlighting the role of biopsy in managing cases.
References
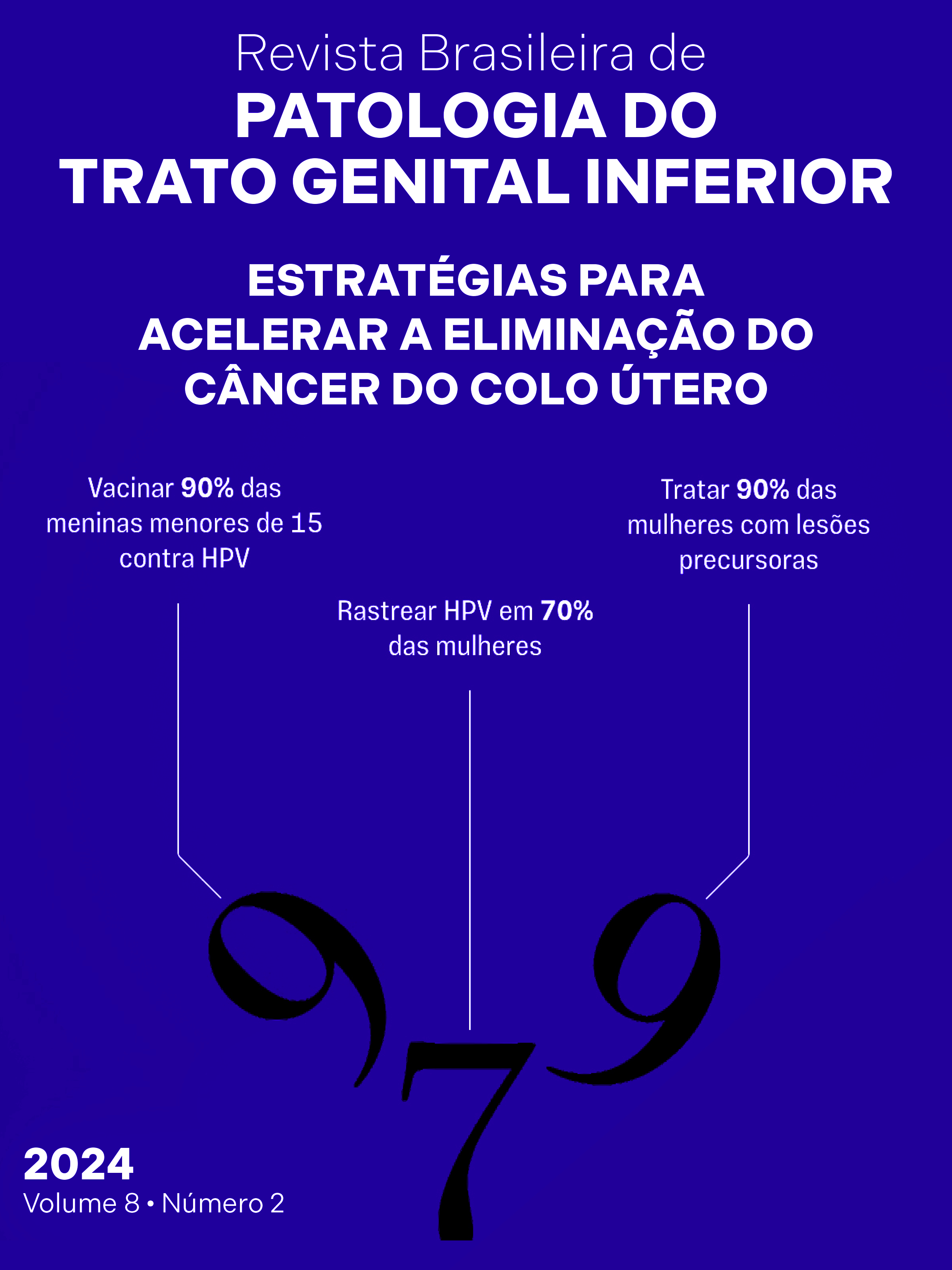
World Health Organization. Global strategy to accelerate the
elimination of cervical cancer as a public health problem [Internet]
Genebra: World Health Organization; 2020 [acessado em 24
novembro 2024]. Disponível em: https://www.who.int/publications/i/
item/9789240014107.
Carvalho CF, Teixeira JC, Bragança JF, Derchain S, Zeferino LC, Vale
DB. Cervical cancer screening with HPV testing: updates on the
recommendation. Rev Bras Ginecol Obstet. 2022;44(3):264-71.
https://doi.org/10.1055/s-0041-1739314
Johns Hopkins Medicine. Cervical biopsy [Internet]. [acessado em 27
novembro 2024]. Disponível em: https://www.hopkinsmedicine.org/
health/treatment-tests-and-therapies/cervical-biopsy#:~:text=A %20
cervical %20biopsy %20is %20a,narrow %20part %20of %20the %20
uterus.
World Health Organization. Cervical cancer: screening and treatment
of pre-cancerous lesions for secondary prevention of cervical cancer.
Technology landscape [Internet]. Geneva: WHO; 2019 [acessado
em 27 novembro 2024]. Disponível em: https://unitaid.org/assets/
Cervical_Cancer_Technology-landscape-2019.pdf
Organização Pan-Americana da Saúde. Câncer do colo do útero
[Internet]. [acessado em 27 novembro 2024]. Disponível em: https://
www.paho.org/pt/topicos/hpv-e-cancer-do-colo-do-utero
Instituto Nacional de Câncer. Mortalidade [Internet]. [acessado em
novembro 2024]. Disponível em: https://www.gov.br/inca/pt-br/
assuntos/gestor-e-profissional-de-saude/controle-do-cancer-docolo-do-utero/dados-e-numeros/mortalidade
Schiffman M, Kjaer SK. Chapter 2: natural history of anogenital
human papillomavirus infection and neoplasia. J Natl Cancer Inst
Monogr, 2003;(31):14-9. https://doi.org/10.1093/oxfordjournals.
jncimonographs.a003476
World Health Organization. WHO technical guidance and
specifications of medical devices for screening and treatment
of precancerous lesions in the prevention of cervical cancer
[Internet]. Geneva: WHO; 2020 [acessado em 27 novembro
. Disponível em: https://apps.who.int/iris/bitstream/
handle/10665/331698/9789240002630-eng.pdf
Bornstein J, Bentley J, Bösze P, Girardi F, Haefner H, Menton M, et al.
colposcopic terminology of the International Federation for
Cervical Pathology and Colposcopy. Obstet Gynecol. 2012;120(1):166-
https://doi.org/10.1097/AOG.0b013e318254f90c
Gage JC, Hanson VW, Abbey K, Dippery S, Gardner S, Kubota J,
et al. Number of cervical biopsies and sensitivity of colposcopy.
Obstet Gynecol. 2006;108(2):264-72. https://doi.org/10.1097/01.
AOG.0000220505.18525.85
Feltmate CM, Feldman S. Colposcopy. UpToDate [Internet]. 2024
[acessado em 26 novembro 2024]. Disponível em: https://sso.
uptodate.com/contents/colposcopy?source=history_widget#H10
Tyagi N, Suneja A, Mishra K, Jain S, Vaid NB, Guleria K. Comparison of
keyes punch biopsy instrument with cervical punch biopsy forceps for
diagnosing cervical lesions. Gynecol Obstet Invest. 2017;82(2):157-
https://doi.org/10.1159/000446948
Girardi F, Reich O, Tamussino K, Burghardt – colposcopia e patologia
cervical: texto e atlas. 4a
ed. Rio de Janeiro: Thieme Revinter; 2017.
Wetcho T, Rattanaburi A, Kanjanapradit K. Quality of tissue from
punch biopsy forceps vs. round loop electrode in colposcopically
directed biopsy: a randomized controlled trial. J Gynecol Oncol.
Robson J, van der Merwe C, Walters L, Noack L, Giles S. The occasional
cervical biopsy. Can J Rural Med. 2022;27(2):72-6. https://doi.
org/10.4103/cjrm.cjrm_13_21
Balan TA, Balan RA, Socolov D, Gheorghiţă VR, Buțureanu TA,
Păvăleanu I, et al. Pregnancy-related precancerous cervical lesions:
pathogenesis, diagnosis, evolution, and impact upon gestation and
fertility. J Clin Med. 2024;13(22):6718. https://doi.org/10.3390/
jcm13226718
Carvalho CF, Teixeira JC, Bragança JF, Derchain S, Zeferino LC, Vale
DB. Rastreamento do câncer do colo do útero com teste de DNA-HPV:
atualizações na recomendação. Femina. 2022;50(4):200-7.
Goidescu I. Cervical biopsy [Internet]. Personal communications.
[acessado em 26 novembro 2024]. Disponível em: https://
abilitatipracticecluj.ro/pdf/eng/Gine_eng_06_Cervical_biopsy.pdf
Foggiatto AI, Carvalho NS, Fonseca FV, Maestri CA. Recurrence in
cervical high-grade squamous intraepithelial lesion: the role of
the excised endocervical canal length-analysis of 2,427 patients.
J Low Genit Tract Dis. 2023;27(1):1-6. https://doi.org/10.1097/
LGT.0000000000000708
Oliveira CCE, Barbosa AMRB. Técnicas de rastreamento e diagnóstico
precoce do câncer de colo uterino [Internet]. [acessado em 27
novembro 2024]. Disponível em: https://